
| Dec. 2015 | |||||||||||
| Top stories | |||||||||||
| In the news | |||||||||||
| Photos | |||||||||||
| Contact us | |||||||||||
| Archive | |||||||||||
|
The global threat of the MERS virus |
This past spring, when an outbreak of MERS — the Middle East Respiratory Syndrome — sickened 186 people and killed 37 in Seoul, South Korea, global public health officials saw this as evidence of the danger of a virus that many see as underestimated so far. In Seoul, the illness was spread from a single person who had come home ill from the Middle East.
The virus is believed to come from contact with camels, but it is spread easily through humans. It’s a relatively new disease — the first recorded case was in 2012 in Saudi Arabia — but it has a high mortality rate: 30 to 40 percent of patients with the disease die.
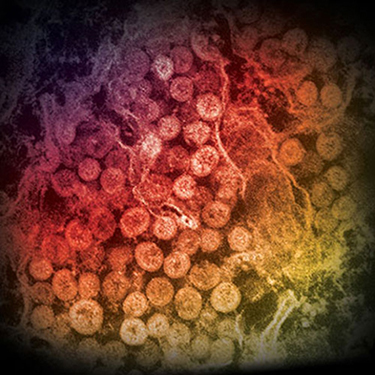
An electron micrograph of a thin section of MERS-CoV, shows the spherical particles within the cytoplasm of an infected cell. Photo courtesy of Cynthia Goldsmith/Azaibi Tamin.
This week [Dec. 13], public health officials are meeting in Seoul to share information about how the virus is spread and how best to respond to it.
Peter Ben Embarek, a MERS expert with the World Health Organization, tells “Here & Now” host Jeremy Hobson why we don’t know a lot about the disease’s course in individuals and how that makes it difficult to develop appropriate treatment.
Information from the WHO on MERS
Interview Highlights: Peter Ben Embarek, scientist with the World Health Organization
Where does MERS come from?
“So, MERS started three years ago. We recorded the first case in Saudi Arabia in 2012. And since then, we have recorded worldwide 1,620 cases of which a good third of them have died. So, a serious disease affecting humans, and this one infected humans by contact with camels.”
It can then pass from human to human, correct?
“Exactly. Once somebody gets it from a camel and goes to a hospital to get treated, sometimes that person is not detected or recognized early on and then has time to pass on the disease to others within the hospital environment typically.”
It might be difficult to tell whether you have MERS because symptoms are common.
“Yes, for some people it’s just a mild disease and you happily recognize it, but if you are one of the susceptible individuals, you may show serious symptoms ranging from pneumonia, respiratory disease, fever, etc. So that’s where you will show up at the hospital or seek treatment with a doctor. And in some cases, still then it can be hard to detect as being a potential MERS case. And therefore, these individuals would not be isolated properly, and that’s where the disease can be transmitted within a hospital environment.”
Not a lot is known about MERS because there haven’t been many autopsies conducted.
“Exactly. Believe it or not, so far out of the 1,620 something cases we have recorded so far, I think only a couple of them have been autopsied.”
Why is that?
“It’s not a tradition in the region and cases that have appeared in other countries have also, for many reasons, not been autopsied. So we don’t really have a good picture of the disease cause within the human individuals, and therefore it’s also difficult to develop appropriate treatments.”
What are the available treatments right now?
“We don’t have specific treatments. So when we have a MERS case, we treat the symptoms. So we would treat the fever, we would treat the pneumonia, we would treat the respiratory distress and then hope that the body will be able to fight off the disease by itself, and it works on young and healthy individuals. But if you’re an elderly person with underlying conditions – diabetes, obesity, chronic respiratory disease and so on – it might not be enough, and so that’s where we see the highest mortality rate.”
This seems like it could be a real threat to the global health community.
“Exactly. It’s one of these diseases that keeps us on the edge and keeps us awake because it has a fairly high mortality rate, as I said, around 30 to 40 percent of the recorded cases have died so far, and that’s to compare to influenza where it’s – depending on the type of influenza and the years – it lies below one percent or around that. So you can see that it’s a very severe and serious disease.”
How do you think the outbreak was handled in South Korea where 37 people died?
“In the beginning, clearly they were overwhelmed. They were not well prepared. They were surprised by this outbreak. And therefore, initially, it looked like it was getting out of control, but quickly they took the matter seriously, put the resources that were needed, isolated all the contacts, introduced proper control within the hospitals, environment and so on. And then, within a few weeks, it was brought under control. But clearly that was a wake-up call not only for Korea, but also for the rest of the world because it showed that even in a very modern, well-functioning health care system, an outbreak like this could bring the whole system down on its knees and cause multiple side effects in terms of economic loss, social distress, et cetera, et cetera. So, very disturbing consequences.”