
| April 2017 | |||||||||||
| Top stories | |||||||||||
| In the news | |||||||||||
| Photos | |||||||||||
| Contact us | |||||||||||
| Archive | |||||||||||
|
Minnesota and Nebraska confirm measles cases |
April 25, 2017 --
The Minnesota Department of Health announced on April 21 a total of nine laboratory-confirmed cases of measles in Hennepin County in southern Minnesota. The department announced the first two cases in this outbreak in the same county on April 12.
Nebraska health officials also reported a case of measles in its western Lincoln County on April 17. This follows a case in the Omaha area that the Department of Health and Human Services announced on March 23.
Iowa Department of Public Health (IDPH) reported on April 24 that there are no known cases in Iowa. It asked health care providers to be vigilant about measles by
- Evaluating the immunization status of all patients and staff to ensure they are up to date with MMR vaccinations.
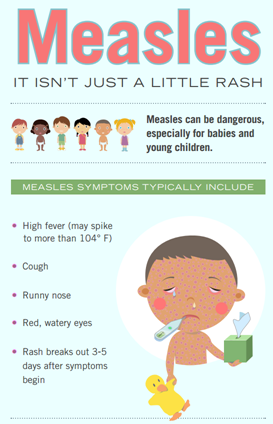
- Considering the diagnosis of measles in patients presenting with febrile illness and clinically compatible symptoms (the "three Cs" - cough, coryza, and conjunctivitis) followed by rash three to five days later. These patients should be asked about recent travel in the U.S., including to locations in Nebraska and Minnesota where recent cases have been confirmed, and international areas with measles cases.
In addition to the case in Nebraska, 21 people from seven states (California, Colorado, Florida, New Jersey, New York, Pennsylvania and Utah) were reported to have measles in the first eight weeks of 2017, according to IDPH. This compares to 70 cases in 2016 and 188 in 2015.
In 2014, the United States experienced 667 cases, the highest number of measles cases since elimination was documented in the U.S. in 2000. Reasons for recent outbreaks include large pockets of unvaccinated people, travelers with measles bringing the disease to the U.S. and a combination of those factors.
CDC provides general information about measles on its website and information about measles vaccination. IDPH publishes the Iowa Acute Disease Monthly Update which contains disease case count information compiled from the Iowa Disease Surveillance System. Visit idph.iowa.gov/CADE and scroll down to "Reports" or access the report directly here.
Developing measles protocols
IDPH provided the following key points for health care providers to help prepare for potential suspect measles cases. Additional resources are in its CADE Epi Manual, including a chapter on measles, as well as fact sheets for the public in English, Bosnian and Spanish.
IDPH recommends:
- All Iowa health care providers and their staff should have had two documented doses of MMR or serologic evidence of immunity to measles.
- During routine office visits, assure that all patients are up-to date on their MMR vaccine.
- Please contact public health immediately to report any Iowans (whether vaccinated or not) who have been possibly exposed to measles to discuss necessary actions.
- When examining a patient with potential measles, health care providers must make arrangements to see the patient in a manner that does not expose others. For example, have the patient come in a back door. Do not allow patients with possible measles to sit in the waiting room. See the patient immediately, document specific onset dates of cough, coryza, fever, rash and initial presentation, and spread of rash.
- Patient presenting with signs of measles (fever, rash, coryza/runny nose, conjunctivitis and cough) should be tested as follows:
Blood Specimen for Serologic Testing (most important specimen to collect):
- Measles IgM test: obtain testing when patient first presents - do not wait. Tests that are negative in the first 72 hours after rash onset may need to be repeated. IgM is detectable for at least 28 days after rash onset.
- Serology-collection: for adults, 4 to 6 ml of blood in a red top or serum separator tube (SST); for infants, 2 to 3 ml of blood in a red top or serum separator tube (SST). Send to the State Hygienic Laboratory on a cold pack, (not frozen) with a completed virus "Serology" test request form.
- If the symptomatic patient has a history of possible disease or vaccination, an IgG test may be appropriate.
Throat Swab:
These specimens should also be obtained when the suspect case first presents to the health care provider.
- RT-PCR for measles and virus culture requires a throat swab, and requires a throat swab collected and placed in separate M4 viral transport media (VTM). The VTM is kept cold and should be sent on a cold pack, (not frozen) with a completed "Viral and Bacterial PCR and DFA Test Request Form." Measles RT-PCR will be sent for testing as appropriate.
- If initial measles testing is positive, viral isolates will be sent to CDC for genotyping. Viral genotyping is an important component of measles surveillance and can help determine the source of the virus (e.g., country of origin).
Shipment of specimens: IDPH will help to arrange immediate transport to the State Hygienic Laboratory for emergency testing to expedite test results.
More information about serology collection is available on the Hygienic Laboratory's website.
Two doses of MMR are required for elementary and secondary school entry in Iowa. The first dose can be given at 12 months of age and the second dose can be administered 28 days later. (However, the second dose is commonly administered as part of the kindergarten shots given between 4-6 years of age.) Generally, persons who started elementary school in Iowa after 1991 and were up-to-date on all school entry vaccine requirements will have received two doses of MMR vaccine.
It is recommended that adults born in 1957 or later receive at least one documented dose of MMR vaccine, or have proof of immunity (measles-IgG positive titer), in order to be considered fully immunized. Any adults who 1) work in a health care facility; 2) plan international travel; or 3) are students in a post-secondary institution, should receive a second dose to be considered fully immunized.
Adults born prior to 1957 are presumed to have had measles and are immune since measles was so common then. However, at least one dose of MMR (or other proof of immunity) is still recommended if they plan to travel internationally or are health care workers.
Vaccination in those who have already had measles or have already received the recommended vaccination is not harmful; it only boosts immunity. Therefore, if someone is unable to verify prior vaccination or prior history of illness, vaccination with MMR is appropriate.